A 40 year old female with palpitations and sob
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 40 year old female who works in the hotel she is aresident of Narketpally came with chief complaints of
Increased heartbeat since 6 months
Breathlessness since 6months
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 6 months back then she developed palpitations which were sudden onset, gradually progressive and develops under stressandheavy work.The palpitations lastsfor 2 to 3 min and relives on rest .But Since last 2 to 3 months she complains of increased frequency and intensity of palpitations making her worry
She also complains of breathlessness ( shortness of breath) since 6 months and it was gradually progressive from grade 1(6months back)to grade 3 (presently like she is getting sob while she was changing her clothes also) and it relieves when she takes rest.
Patient also has occasional dizziness and headache when there is delay in food intake or prolonged standing and it gets relieved on taking rest or food.
PAST HISTORY
Not a known case of Diabetes, Hypertension, Asthma, Tuberculosis,Epilepsy, Thyroid disorders.
She has acidity from past 15 years back
She develops burning sensation in abdomen when she consumes oily food, spicy foods, and chapati.And for this she takes omeprazole every morning half n hr before food.
7 years back She had severe vomitings and diarrhea for which she went to gastroenterologist and got endoscopy colonoscopy done and was diagnosed with irritable Bowel syndrome she then took medication for one year.
After that since she has acidity she takes medications to reduce her acidity which are not prescribed by doctor
No history of prolonged hospital stay or surgeries.
She had sore throat 2 months back for which she consulted Local RMP and was given some IV medication and was asked to get thyroid function test and complete blood picture done. Her thyroid profile was normal but her HB was 5.5 gm/dl.(anemic)
The local practitioner gave some oral medications for anemia but she neglected it .
TREATMENT HISTORY Using pantop since 15 years every day morning
FAMILY HISTORY
No relevant family history
MENSTRUAL HISTORY
Menarche at 13 years
Regular cycle , 3/28
Uses 2 pads/day
Not associated with clots
No pain
Has premenstrual symptoms like back pain, leg pain
PERSONAL HISTORY
DAILY ROUTINE
She wakes up at 6.30 am gets fresh up
Does household work( sweeping, cleaning dishes,cooking)
She takes her breakfast at 8.30 am
From 9 am to 2pm she starts preparing items like cutting vegetables and cleans tabels and cleans the hotel and she sits in the counter
She takes her lunch at 2pm
And from lunch to dinner she sits in the counter and at 5pm she drinks tea
At 9pm she eats her dinner
From 9pm to 10pm she does hotel work ( cutting vegetables, serves people, cleans hotel, cleans dishes)
Returns to home by 10 or 11 pm
Sleeps by 11 pm
Diet -vegetarian
Appetite- normal
Bowel and bladder movements-regular
Sleep-adequate
Addictions- no addictions
Allergies -no addictions
GENERAL EXAMINATION
Patient was conscious,coherent, cooperative
Well oriented to time, place ,person
Poorly built and poorly nourished
height- 5.2 inch
Weight-44 kg
BMI- 17.7
Pallor - present
Icterus- absent
Cyanosis -absent
Clubbing-absent
Lymphadenopathy -absent
Edema-absent
VITALS
Temperature -a febrile
BP- 130/90 mmhg RR- 16cpm
PR- 84bpm
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
Inspection :
Abdomen flat
Moves with respiration
no abdominal distension
umbilicus is central and inverted
no engorged veins
no scars,sinuses,
hernial ornifices are clear
Palpation
All inspectory findings are confirmed
No tenderness in the abdomen
Percussion
No significant findings
Auscultation
Bowel sounds heard
No bruits
RESPIRATORY EXAMINATION
Trachea central
Normal vesicular breath sounds Heard
Bilateral air entry present.
CARDIOVASCULAR SYSTEM
S1S2 heard
No murmurs
CENTRAL NERVOUS SYSTEM
No focal neurological deficits
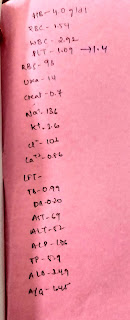
Investigations:
PROVISIONAL DIAGNOSIS
Dimorphic anemia
Secondary to nutritional cause
IDA?
Folate deficiency anemia?
TREATMENT
On 29/11/22
Inj Vitcofol 1.5gm IV OD in 100 ml NS
Tab albendazole 400 mg PO OD
Tab Lirogen PO OD every alternate day
Tab esomeprazole 20mg PO OD (7am)
Vitals monitoring every 6th hrly
On 30/11/22
Inj Vitcofol 1.5gm IV OD in 100 ml NS
Tab Livogen IM PO OD every alternate day
Tab esomeprazole 20mg PO OD (7am)
Vitals monitoring every 6th hrly.























Comments
Post a Comment